Irritable Bowel Syndrome (IBS): The Latest Science on an Under-Diagnosed Disorder
September 12, 2022
By: Corrie Fletcher
Categories: Nutrition & Diet
IBS is a disorder of gut-brain interaction that ranges in severity from mild and intermittent to severe and continuous.
Let’s talk about your belly ache.
Are you a silent sufferer, wondering if you should see your doctor? Sometimes it’s hard to know what is normal, what can safely be ignored, or if a doctor can even help. If you have chronic or recurring stomach pain, cramping, bloating, nausea, constipation and/or diarrhea, you may have a real and treatable disorder called IBS. It is estimated that 10-15% of the United States population suffers from IBS. It is one of the most common gastrointestinal disorders seen by doctors, yet 55-75% of sufferers unnecessarily go through life undiagnosed.2
What exactly is IBS?
IBS is a disorder of gut-brain interaction that ranges in severity from mild and intermittent to severe and continuous.7 It is not a disease, and unlike many other conditions that can affect the GI tract, it rarely causes permanent damage.9 However, IBS can negatively impact quality of life, causing many of those who suffer from it to miss work and important social events. Food anxieties may cause sufferers to eliminate various foods, putting them at nutrition risk. Symptoms typically begin between the ages of 20 and 50.6 IBS is characterized by abdominal discomfort and altered bowel habits, but symptoms unrelated to the intestines are also commonly correlated with IBS. (See list below.)
Common IBS Symptoms
Abdominal discomfort
- Sharp Pain
- Bloating
- Cramping
- Fullness
- Nausea
- Burning
Altered bowel habits
- Constipation
- Diarrhea
- Mucus in the Stool
Other correlated symptoms
- Stress, anxiety, or depression
- Fibromyalgia-like symptoms
- Bladder symptoms
- Fatigue
- Headaches
- Sleep disturbances
Getting a proper diagnosis
Currently, there is no reliable diagnostic test for IBS. If tests are run to rule out other diseases, the intestines will appear healthy, and there will be no sign of disease.10 Thus, a doctor will diagnose IBS based on symptoms. There are four different subtypes of IBS.
IBS Subtypes
- IBS-C: Constipation predominant
- IBS-D: Diarrhea predominant
- IBS-M: Mixed
- IBS-U: Unspecified
Causes and Triggers
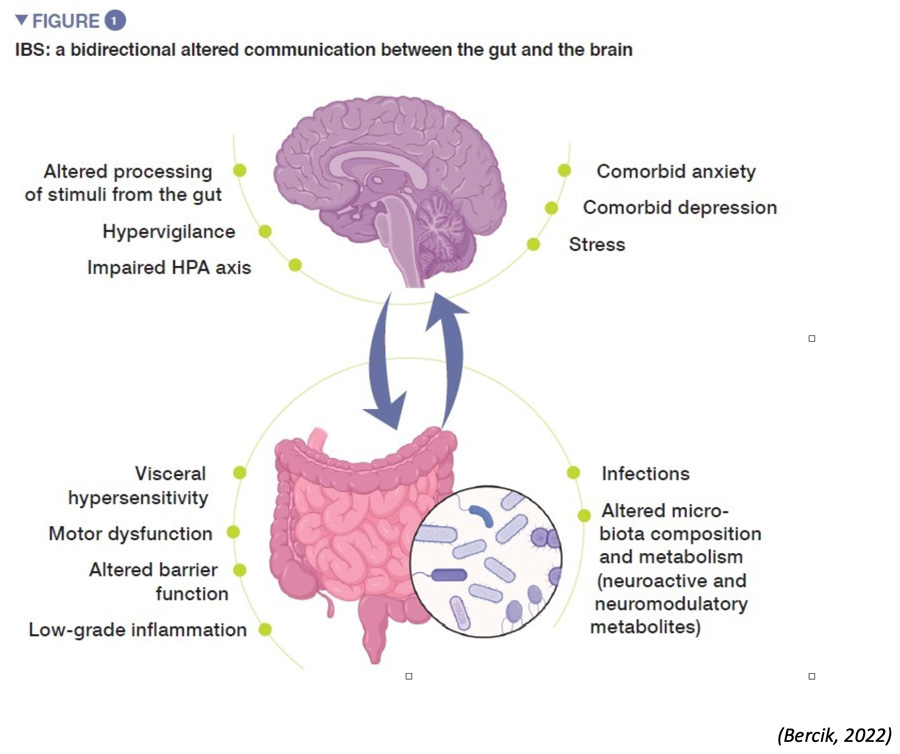
According to the American College of Gastroenterology, “We do not really know what causes IBS. We do think that it is due to problems with how the bowels work. In recent years, we have discovered certain chemicals in the gut which send signals from the intestines to the brain. Learning about these has helped make pills to treat IBS. We do think that IBS can be due to problems that continue after people have had a bowel infection.
We also think that it could be because of the overgrowth of normal good bugs or getting bad bugs growing in the gut. It does not seem like IBS comes from food intolerance or allergies” (2022). Food intolerances can, however, trigger a recurrence of IBS symptoms.5 Although the cause of IBS is not completely understood, many triggers have been identified, like stress, erratic eating behaviors, and physical inactivity, to name a few.
Likely Underlying Mechanisms of IBS
Management of Symptoms
The management of IBS symptoms is often multifactorial. Your gastroenterologist may refer you to a dietitian or possibly even a psychiatrist.2 Each subtype of IBS requires a different treatment plan. Each individual also has a different set of triggers, and symptoms often do not immediately follow the trigger, so it is beneficial to work closely with your provider to help you identify your triggers and establish a treatment plan. The process may be touch-and-go and can take multiple visits, but it is well worth it.
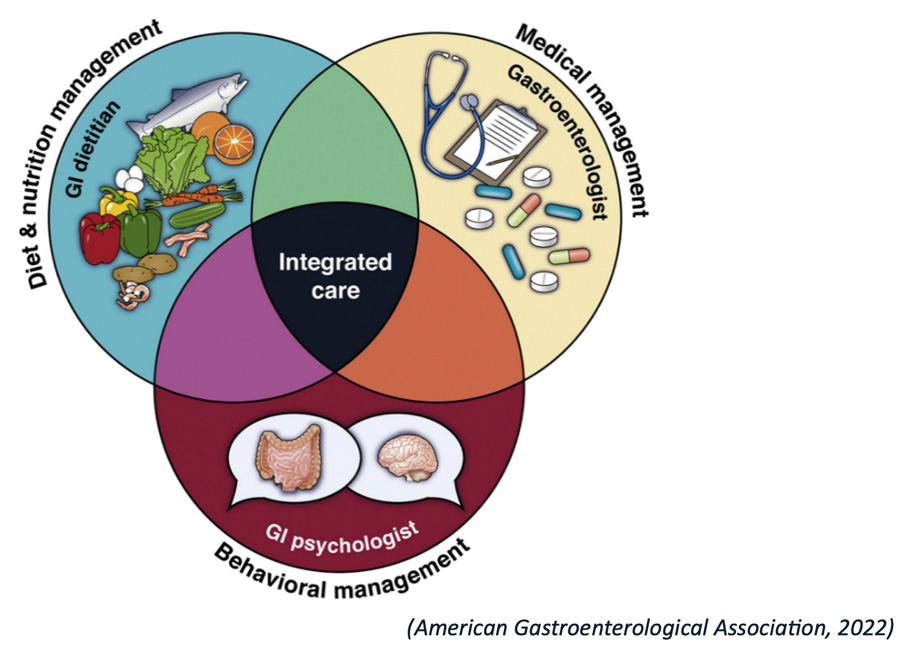
Medical management
- Over-the-counter or prescription drugs for constipation or diarrhea
- Probiotics
- Antibiotics
- Antidepressants
- Anti-spasm drugs
Diet and nutrition management
- Diet and meal regularity1
- Avoid sudden changes in your diet.
- Try not to eat too fast, overeat, or go too long between meals.
- Sit down and relax when you eat.
Monitor these macronutrients for sensitivity:
Fiber
- Aim for a steady 20-35g per day.7
- If increasing fiber intake, choose soluble fiber.11
- Soluble fiber maintains stool consistency and eases passage.
- High amounts of insoluble fiber may irritate the large intestine.11
Fat: High-fat meals may trigger intense gastro-colic reflexes.8
Carbohydrates1
- High fructose beverages, like apple juice and soda
- Sugar alcohols, like sorbitol, xylitol and mannitol
- Lactose, if intolerant
- FODMAP (fermentable oligo-di and monosaccharides and polyols) foods, if intolerant
Fluids: Consume 48–64 oz of liquids per day.1
Keep a food journal to help you and your provider identify your triggers. An elimination diet may be helpful.1 Eliminating foods from your diet can put you at nutrition risk. These diets are meant to be short-term and should follow strict protocols to be effective, so it is best to work closely with your gastroenterologist or dietitian.
Behavioral Management3
- Cognitive-behavioral treatment
- Stress management
- Meditation
- Other relaxation methods
- Exercise improves gut function
Connect with a Registered Dietitian
References
1. Academy of Nutrition and Dietetics. Nutrition Care Manual®. Irritable Bowel Syndrome: Nutrition Intervention. Version current 2022. https://www.nutritioncaremanual.org (accessed 21 August 2022).
2. American College of Gastroenterology. Irritable bowel syndrome. Version current 21 March 2022). https://gi.org/topics/irritable-bowel-syndrome/ (accessed 21 August 2022).
3. American Gastroenterological Association. Irritable Bowel Syndrome. Version current n.d. https://patient.gastro.org/irritable-bowel-syndrome-ibs/ (accessed 21 August 2022).
4. Bercik, P. Microbiota gut-brain axis in irritable bowel syndrome. Biocodex Microbiota Institute. Version current 13 October 2021. https://www.biocodexmicrobiotainstitute.com/en/pro/microbiota-gut-brain-axis-irritable-bowel-syndrome (accessed 21 August 2022).
5. Crowe, S. Food allergy vs food intolerance in patients with irritable bowel syndrome. Gastroenterology and Hepatology. Version Current January 2019. https://www.gastroenterologyandhepatology.net/archives/january-2019/food-allergy-vs-food-intolerance-in-patients-with-irritable-bowel-syndrome/ (accessed 21 August 2022).
6. Hopkins Medicine. Irritable Bowel Syndrome (IBS). Version current n.d. https://www.hopkinsmedicine.org/gastroenterology_hepatology/_docs/_pdfs/small_large_intestine/irritable_bowel_byndrome_IBS.pdf (accessed 21 August 2022).
7. International Foundation for Gastrointestinal Disorders. About IBS. Version current 2022. https://aboutibs.org/what-is-ibs/what-causes-ibs/ (accessed 21 August 2022).
8. Monash University. Starting the FODMAP diet. Version current n.d. https://www.monashfodmap.com/ibs-central/diets/ (accessed 21 August 2022).
9. National Institute of Health. Irritable bowel syndrome. Version current November 2017. https://www.niddk.nih.gov/health-information/digestive-diseases/irritable-bowel-syndrome (accessed 21 August 2022).
10. National Health Service. Irritable bowel syndrome. Version current 24 February 2021. https://www.nhs.uk/conditions/irritable-bowel-syndrome-ibs/getting-diagnosed/#:~:text=There%27s%20no%20test%20for%20IBS,and%20inflammatory%20bowel%20disease%20(IBD) (accessed 21 August 2022).
11. Oregon State University. Fiber. Versions current 2019. https://lpi.oregonstate.edu/mic/other-nutrients/fiber (accessed 21 August 2022).
About the Author
Corrie Fletcher is an intern with St. Mary’s Food and Nutrition Department. She has her Bachelors of Science degree in Nutrition and is currently in the Gulf Coast Dietetic Internship, which is a supervised practice program required to sit for the Registered Dietitian exam.
