Neurointerventional Biplane

Neurointerventional Biplane brings state-of-the-art care to Northeast Georgia
St. Mary’s provides leading-edge technology for the diagnosis and treatment of stroke, brain aneurysms, brain and neck tumors, and other neurological conditions. Our neurointerventional biplane angiography system produces highly detailed, three-dimensional views of blood vessels leading to the brain and deep within the brain. It’s fast, highly accurate and painless.
The biplane represents a giant leap in helping physicians diagnose neurological abnormalities and then treat them with endovascular procedures. Endovascular procedures are minimally invasive, which means they do not require large surgical incisions. Instead, these procedures use very small, specialized instruments that are inserted into a large blood vessel in the upper leg through a small “port”. The instruments are then threaded through the inside of blood vessels to reach targets in the brain and neck.
The system is called a biplane because it produces x-ray images simultaneously from two angles: from front to back and from side to side. This creates pinpoint accuracy while reducing the amount of contrast material required by older systems. It improves visualization of diagnostic and therapeutic procedures and shortens the time it takes to complete a neurological angiogram.
The images produced by the biplane system aid physicians in performing neurointerventional procedures such as:
- Mechanical thrombectomy (MT) – blood clot removal for emergency treatment of strokes caused by large vessel occlusions
- Aneurysm repair and the treatment of arteriovenous malformations
- Carotid artery blockage removal
- Brain and neck tumors removal
- Intracranial hemorrhage repair
- Spinal compression fracture repair
- Refractory epistaxis treatment

3D image of a brain aneurysm (shaded in blue)
For many patients, neurointerventional biplane procedures can replace an “open” procedure, resulting in a shorter hospital stay, quicker recovery time, reduced pain and less risk of complications. For stroke patients with large-vessel blockages, the biplane offers a form of treatment that is not possible with any other system or through open surgery.
The biplane is a multi-use piece of equipment and can also be utilized by St. Mary’s board-certified cardiologists for heart and blood vessel procedures such as angioplasty and electrophysiology.
Neurointerventional biplane technology in our region is available only at St. Mary’s Hospital.
Frequently Asked Questions
Why is this equipment important to our community?
The neurointerventional biplane has taken our already nationally recognized stroke care program to the next level by bringing cutting edge technology to serve our patients.
Currently, there are only four other neuro-biplanes in Georgia: three in Atlanta and one in Augusta. Without the biplane at St. Mary’s, patients requiring emergency neurointerventional care would face an expensive and weather-dependent life-flight to Atlanta or Augusta. Even by helicopter, transport would extend the time it takes to restore blood flow to the brain, resulting in potentially more disability and worse outcomes. Non-emergency patients would have to receive care farther from home, which can be a burden on loved ones and may require expensive and stressful city-to-city medical transportation.
Why is St. Mary's Stroke Center recognized among the best?
St. Mary’s provides 24/7 mechanical thrombectomy care and is the first hospital in Georgia to be certified by The Joint Commission as a Thrombectomy-Capable Stroke Center. St. Mary’s has been identified as one of the best stroke centers in the nation and has been advancing its stroke program since 2002, when our Center for Rehabilitative Medicine opened. St. Mary’s serves as a hub for rural hospitals in surrounding communities and has the staffing and infrastructure to support biplane services, including a dedicated Neurosciences Critical Care Unit and neurological hospitalists – specialists who practice only in the hospital setting – who provide 24/7 coverage for our neurological patients.
Who are St. Mary’s neurointerventional specialists?
Dr. Neil Woodall joined Georgia Neurological Surgery (GNS) in August 2017. Dr. Woodall has Fellowship Training in cerebrovascular and skull-based surgery. He received his training at the prestigious Barrow Neurological Institute (BNI) in Arizona, which trains only two physician fellows per year. Dr. Woodall is from Columbus, Georgia, attended the University of Georgia and earned his medical degree from the Medical College of Georgia in Augusta
Dr. Feroze Afzal joined GNS in August 2021. A vascular neurologist, he came to GNS and St. Mary’s from Augusta University, where he served as stroke director for University Hospital from 2016-2019 before entering his fellowship in neuroendovascular medicine. Dr. Afzal completed his internal medicine internship at Metropolitan Hospital Center in New York, and his neurology residency and neurovascular fellowship at Augusta University.
How many stroke patients per year does St. Mary's currently see and how many could benefit from biplane technology?
St. Mary’s biplane was introduced in 2017 and has already touched thousands of patients. Typically, St. Mary’s sees between 300 and 400 active stroke patients every year. Of those active stroke patients, 15% receive the clot busting medication tPA (Alteplase) to try to dissolve the clot and restore blood flow. Many have large-vessel blockages and are also eligible for MT. We anticipate that as many as 70 MT procedures could be performed in the first year.
Why do so few stroke patients receive Alteplase?
Two reasons: First, Alteplase is only effective if given within about 3 hours of the onset of symptoms. It can save brain cells that are stressed by the stroke, but it cannot revive cells that have already died. Once most of the stressed cells have died, Alteplase does not help. So patients who have a stroke in their sleep or who don’t seek care right away may get to the hospital too late for Alteplase to be effective. This is why it is essential to call 911 the moment stroke symptoms appear.
The second reason is that Alteplase works by dissolving the blood clots that cause most strokes. But about 10-15% of strokes are caused by a torn blood vessel. In these cases, Alteplase would make it harder for doctors to stop the bleeding and would actually worsen the stroke. CT imaging is used to determine if it is safe to administer Alteplase.
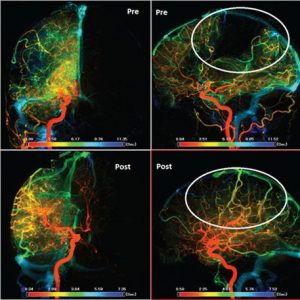
Is it possible to see if treatment is working?
Yes. Before-and-after CT images are used to visualize the effect of treatment.
- Top. Before: the circled dark area shows where blood flow to part of the brain has been blocked by a blood clot in a major blood vessel. The brain cells in this dark area will die unless blood flow is quickly restored.
- Bottom. After: MT has restored blood flow to the affected area of the brain, saving millions of brain cells and reducing the patient’s risk of death or disability.